The banded krait, a primarily nocturnal Southeast Asian reptile, produces and envenomates with a highly lethal compound that irreversibly and with great affinity binds to nicotinic acetylcholine receptors (nAChRs). As a result, it competes with acetylcholine (ACh) for the receptor, and stays there, exerting its deadly neurotoxic effect. Do you see how this relates to train-of-four monitoring yet? Let’s get into it.

| Table of Contents:
Venom casts light on neuromuscular transmission
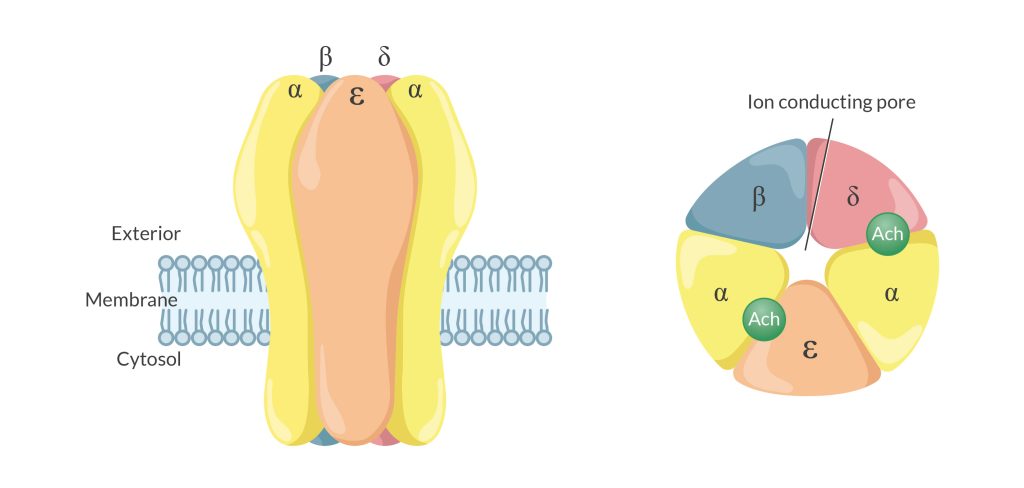
Nondepolarizing muscle relaxants (NDMRs) target nAChRs, with ACh acting at the two α-subunits on the receptor. The krait’s venom, α-bungarotoxin, has a long record of utility in identifying, quantifying, and assaying nAChRs. Much of what we know about those receptors and how NDMRs work is due to what this potent venom reveals in lab research. Who could have imagined that a venomous reptile would help illuminate normal human physiology?
Like the sheer lethality of α-bungarotoxin in the natural world, the NDMRs used in our daily clinical work may be the most dangerous, intentionally administered drugs on planet Earth. Without tools that help guide their administration, considerable uncertainty may exist about the safe and effective dosing of NDMRs in clinical practice.
Reducing uncertainty: The role of Train-of-Four Monitoring
As with most things in life, timing is essential. Train-of-Four (TOF) monitoring offers real-time insight into assessing the onset, duration, and offset of NDMRs. But how does it do that? What’s good to know?
Imagine the uncertainty of driving without a speedometer, flying without an altimeter, baking not knowing the oven temperature, or judging SpO2 without an oximeter. Technology, simple or complex, is used in each of these scenarios to guide our decision-making. Likewise, we have the technology to reveal the degree of block induced by NDMRs.
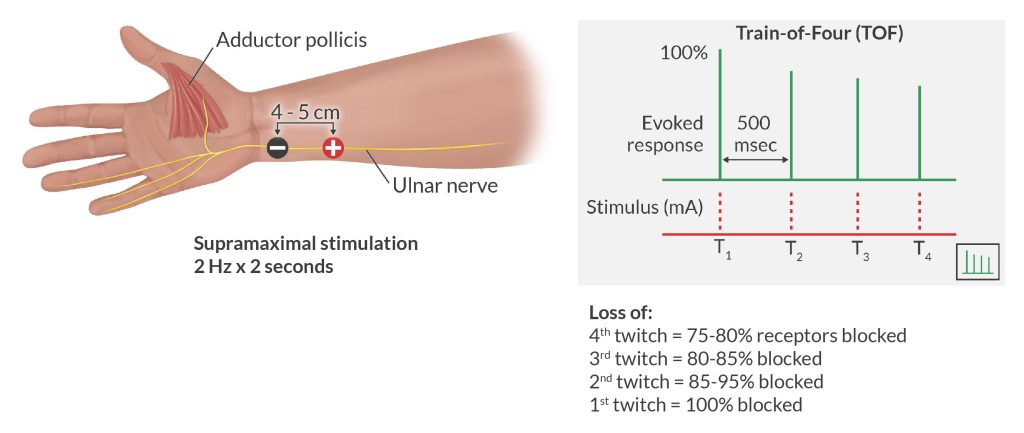
Introduced into clinical practice in the 1970s, the TOF sends 4 brief electrical impulses to a peripheral nerve at 2 Hertz (Hz = cycles per second). That plays out as 4 stimuli over 2 seconds. The response is observed in the associated innervated muscle. As the neuromuscular block intensifies, there is a progressive decrease in the amplitude of the twitches and the disappearance of the 4th, then 3rd, then 2nd, and finally, the 1st twitch.
By counting the twitches present, or absent, we can estimate the percentage of blocked nAChRs. Analyzing what is observed by sight or feel, one can construct a TOF ratio, which is the strength (or amplitude) of the 4th twitch to the 1st twitch. As that ratio decreases, there is evidence of increasing NDMR-induced paralysis.
Using TOF to measure anesthesia recovery
Though some rely entirely on their experience to dose NDMRs, many of us use visual/touch assessment of the TOF to titrate NDMRs and to assess reversal. Clinical signs to assess recovery, such as head lift, grip strength, and teeth clenching, are of minimal value and can be misleading.
Visual/tactile observation of TOF fade is a highly specific indicator of residual paralysis but has a very low sensitivity as humans fail to detect fade when the TOF ratio is >0.3 to 0.4. The current and widely accepted consensus is that sufficient recovery of nAChR blockade is a TOF ratio of ≥0.9.
Post-operative residual block (PORB): uncertainty no more!
Why 0.9 you ask? There is abundant evidence, no longer uncertain, that PORB is extremely common, occurring in 40% or more of patients dosed with NDMRs. Similarly, many of us do not appreciate the enormous patient variability in the duration of a NDMR. This is important because PORB is associated with a patient experiencing distressing signs of weakness, dysphagia, risk of airway obstruction, blunted hypoxic ventilatory response, and concerns about aspiration. Let’s avoid uncertainty: monitor appropriately using the TOF!
A better alternative: quantitative TOF Monitoring
Despite the availability of quantitative TOF instruments, these have not been widely adopted. The value of quantitative measurement is that it eliminates our subjective interpretation of nAChR blockade, instead displaying sophisticated machine-generated information. Recently introduced devices are small, reliable, and relatively inexpensive. We may be on the same utilization trajectory that we were for the pulse oximeter in the late 1980s.
The most recent practice guidelines
While practice guidelines are not intended as absolutes or standards of care, they provide basic recommendations that are supported by the most recent best evidence. However, the first is an AANA Standard of Care:
- When using NDMRs, monitor neuromuscular response
- Avoid using clinical assessment alone to prevent PORB
- Use quantitative TOF monitoring in favor of qualitative monitoring to guide administration and avoid PORB
- Use quantitative monitoring to confirm TOF ≥ 0.9 before extubation. Be aware that TOF ≥ 0.9 does not guarantee avoidance of PORB.
- Use the ulnar nerve and adductor pollicis muscle for TOF monitoring. Avoid using the eye muscles as they are undependable and the adductor pollicis recovers slower than the eye muscles
- To avoid PORB and using TOF as your guide, sugammadex is recommended over neostigmine to reverse deep, moderate, and shallow depth of block caused by rocuronium or vecuronium.
- Using TOF as your guide for atracurium or cisatracurium, use neostigmine at a low level of block depth[DF1], allowing at least 10 minutes before extubation.
Of the many drugs that we use in caring for our patients, muscle relaxants have a particularly dangerous profile. Advances in our understanding of how they work, much of which came from a venomous snake, and the introduction of TOF technologies permitting quantification of block depth, have reduced uncertainty associated with dosing NDMRs. In doing so, patient safety benefits.
As CRNAs ourselves, we understand the challenge of fitting CRNA continuing education credits into your busy schedule. When you’re ready, we’re here to help.






