When breathing difficulties arise, the ASA (American Society of Anesthesiologists) Difficult Airway Algorithm becomes a critical tool. Let’s explore this decision-making framework and understand how it helps ensure patient safety during procedures.
| Table of Contents:
-
- Airway Management Isn’t Becoming Safer
- Pre-Induction Decision Tool: Awake vs. Asleep Airway Management
- New ASA Difficult Airway Algorithm Infographics
- Optimize Oxygenation, Always
- Capnography Remains the Gold Standard for Assessing Ventilation
- Situational Awareness and Limiting Attempts
- 2022 ASA Difficult Airway Algorithm Walkthrough
- Focus on Extubation
- New ASA Pediatric Difficult Airway Algorithm
Airway management in anesthesiology isn’t becoming safer
Given the vast array of new airway devices on the market, you might assume that airway-related morbidity and mortality are on the decline. Sadly, the evidence doesn’t bear this out. While the frequency of airway incidents remains unchanged, patient outcomes are getting worse. Why? The most likely explanations include:
- Judgment errors
- System errors
- Not progressing to a surgical airway soon enough
- Possibly incorporating new airway devices into practice (devices that users may not have adequate experience with)
The updated 2022 ASA Difficult Airway Algorithm addresses these issues. Let’s examine the highlights.
Pre-induction decision tool: awake vs. asleep airway management
The 2022 algorithm includes a decision tree to help you choose between an awake or post-induction airway management strategy.
Remember that the risks of awake intubation are quite low, while the potential risk of dealing with a difficult airway in an unconscious, possibly paralyzed patient is enormous. The “can’t ventilate, can’t intubate” scenario is the most dreaded of scenarios.
Consider awake intubation if you expect difficulty with laryngoscopy or intubation plus any of the following 4 things:
- Difficult facemask ventilation
- Difficult supraglottic airway placement
- Aspiration of gastric contents
- Apnea intolerance
New ASA difficult airway algorithm infographics
Cognitive aids guide decision-making, and the 2022 ASA Difficult Airway Algorithm includes 4 infographics you can use at the bedside in real time. The infographics use color coding to indicate whether you can ventilate the patient or not. It’s important to note potential accessibility issues in those with color blindness. If staffing permits, it’s helpful for a dedicated person to read the algorithm as airway management progresses.
Optimize oxygenation, always
While giving oxygen may seem obvious, the task force identified a need to strongly emphasize optimizing oxygenation throughout airway management. Indeed, research and clinical experience show that, in the heat of the moment, focusing on task completion can distract from this most basic responsibility (i.e., remembering to give oxygen to the patient).
You can optimize oxygenation in 2 ways:
- Administer oxygen via high- or low-flow nasal cannula. Turn it on before you begin airway management and continue it the entire time you manage the airway – this includes extubation.
- Place the patient in a head-elevated position to maximize FRC by unloading the diaphragm.
Capnography remains the gold standard for confirming ventilation
The algorithm stresses the measurement of exhaled carbon dioxide to verify gas exchange. Pulse oximetry is not a suitable monitor of airway patency due to the time delay between loss of airway patency and arterial oxygen desaturation.
Situational awareness and limiting attempts
A fixation error occurs when you focus on a single part of a process at the expense of other, often more important, aspects. During a dire airway situation, it’s easy to fixate on securing the airway while neglecting other critical tasks (e.g., ensuring oxygenation). Ignoring the passage of time through repeated failed attempts consumes precious time as the CNS tissue suffers from a rapid decline in oxygen delivery. Anoxia can cause brain damage in as little as 4 minutes and leads to death only 4 – 6 minutes later.
So, how many attempts are reasonable? It’s reasonable (but not required) to limit attempts with any airway class (i.e., facemask, SGA, intubation) to 3 attempts + 1 more attempt by a clinician with higher skills. This is NOT a strict rule; the “best” answer changes with each unique clinical situation, provider skillset, and available resources.
The emphasis on situational awareness and limiting attempts prompts clinicians to consider a surgical airway sooner than they otherwise might. Failure is not having to resort to a surgical airway. Rather, failure is not resorting to a surgical airway soon enough!
2022 ASA difficult airway algorithm walkthrough
Practicing the algorithm is the best way to master it.
We created an interactive version where you can quiz yourself on your treatment options at key points in the pathway. As an aside, the new algorithm states that combining techniques can enhance success. For instance, there’s a greater first-time success rate when using a video laryngoscope in conjunction with a flexible bronchoscope.
There’s no better way to learn the 2022 ASA Difficult Airway Algorithm than by exploring it for yourself. Click the Start button below to review the algorithm. Also, you can click the numbers to reveal your airway management options at each step of the process.
Focus on extubation
Transitioning to extubation after a difficult airway deserves consideration, and the new algorithm provides greater clarity on this topic. Consider a temporary device, such as an airway exchange catheter, to facilitate re-intubation should the need arise. These devices contain a lumen that you can use to monitor end-tidal CO2, insufflate oxygen, or jet ventilate. Alternatively, you could place a conduit for reintubation, such as a supraglottic airway. Consider the best location to extubate as well as available resources and personnel.
You must communicate the nature of airway difficulty to the patient and clearly document it in the patient record. Finally, you should encourage the patient to register with an emergency notification service.
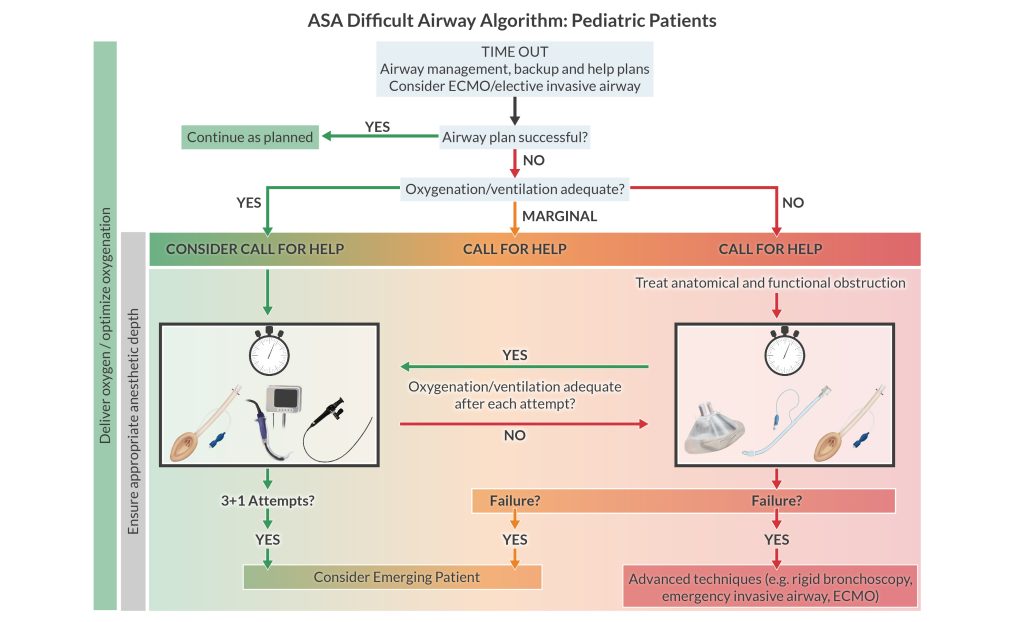
Pediatric algorithm
In 2022, the ASA Difficult Airway Algorithm introduced a pathway for children for the first time. Here are the most notable aspects:
-
- Consider ECMO early.
- Limit attempts, be situationally aware, and optimize oxygenation.
- Consider rigid bronchoscopy (by someone trained in the technique).
- The algorithm discourages using an airway exchange catheter at extubation due to the risk of airway injury and pneumothorax.
Knowledge of these guidelines will give you the confidence to keep your patients safe in what may be the most taxing moments in your career. In contrast to previous versions, the 2022 ASA Difficult Airway Algorithm places greater emphasis on patient safety and outcomes (beyond securing the airway). This represents a not-so-subtle change in thinking that we applaud. Your patient, and their loved ones, will thank you.
Your action plan
-
- Before your next case, walk through the algorithm in your mind. If you get stuck, return to this page to brush up on our interactive algorithm. ☝️
- Read the complete 2022 ASA Difficult Airway Algorithm.
Want to earn Class A credits while staying up to date on current anesthesia practice? Check out our CPC Core Modules and CRNA Updates courses.